The Role of Diet and Exercise in Diabetes Management

Mastering Diabetes: The Holistic Approach
Diabetes is a chronic condition that affects millions of people worldwide, characterized by elevated levels of blood sugar. While genetics and other factors play a role, lifestyle choices, particularly diet and exercise, have a significant impact on its management. Managing diabetes effectively requires a comprehensive approach, and integrating a balanced diet and regular exercise routine are crucial components.
Dietary Considerations
The foods we consume directly influence blood sugar levels, making dietary choices a cornerstone of diabetes management. Here are some key considerations:
Carbohydrate Management:
Carbohydrates have the most significant impact on blood sugar levels. For individuals with diabetes, monitoring carbohydrate intake and choosing complex carbohydrates with a low glycemic index (GI) can help stabilize blood sugar levels. Foods like whole grains, legumes, fruits, and vegetables are excellent choices.
Portion Control:
Controlling portion sizes helps manage calorie intake, which is vital for weight management and blood sugar control. Monitoring portion sizes of carbohydrates, proteins, and fats can prevent blood sugar spikes and promote overall health.
Healthy Fats:
Incorporating healthy fats such as those found in avocados, nuts, seeds, and fatty fish can improve insulin sensitivity and support heart health. However, moderation is key, as fats are calorie-dense and can contribute to weight gain if consumed excessively.
Fiber-Rich Foods:
Foods high in fiber, such as fruits, vegetables, whole grains, and legumes, help regulate blood sugar levels by slowing down digestion and absorption. Additionally, fiber promotes satiety, aiding in weight management and reducing the risk of heart disease.
Limiting Sugary and Processed Foods:
Foods high in added sugars and refined carbohydrates should be limited or avoided as they can cause rapid spikes in blood sugar levels. Processed foods, sugary beverages, and sweets offer little nutritional value and can contribute to weight gain and insulin resistance.
Regular Meal Timing:
Consistency in meal timing helps stabilize blood sugar levels and prevents extreme fluctuations. Eating smaller, balanced meals/snacks throughout the day can help maintain steady energy levels and prevent overeating.
Exercise and Physical Activity
In addition to dietary modifications, regular exercise plays a crucial role in managing diabetes. Here’s how:
Improved Insulin Sensitivity:
Physical activity helps cells become more sensitive to insulin, allowing for better glucose uptake and utilization by the body. This can lead to more stable blood sugar levels and potentially reduce the need for medication in some individuals.
Weight Management:
Exercise helps burn calories and build lean muscle mass, aiding in weight loss or maintenance. Maintaining a healthy weight is essential for managing diabetes, as excess body fat can increase insulin resistance and the risk of complications.
Cardiovascular Health:
Diabetes increases the risk of cardiovascular diseases such as heart attack and stroke. Regular exercise strengthens the heart, improves circulation, and lowers blood pressure and cholesterol levels, reducing the risk of heart disease.
Stress Reduction:
Exercise is a natural stress reliever and can help lower cortisol levels, which can contribute to better blood sugar control. Managing stress is essential for overall health and diabetes management.
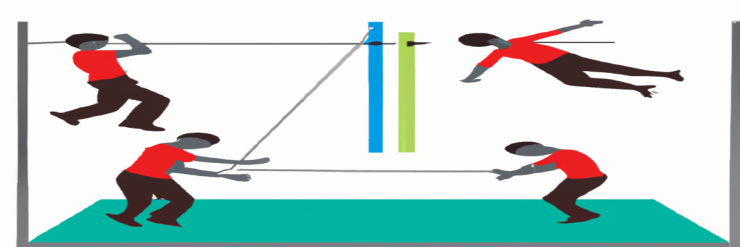
Types of Exercise:
A combination of aerobic exercise (such as walking, cycling, swimming) and strength training is recommended for individuals with diabetes. Aerobic exercise helps improve cardiovascular health and blood sugar control, while strength training builds muscle mass and improves metabolism.
In addition to diet and exercise, there are other important aspects to consider in diabetes management:
Medication Adherence:
For many individuals with diabetes, medication such as insulin or oral hypoglycemic agents is necessary to maintain optimal blood sugar levels. Adhering to prescribed medication regimens as directed by healthcare professionals is essential for effective management.
Regular Monitoring:
Monitoring blood sugar levels regularly allows individuals to track their progress, identify patterns, and make necessary adjustments to their treatment plan. This may include self-monitoring with glucose meters or continuous glucose monitoring (CGM) systems.
Education and Support:
Education about diabetes and its management is crucial for empowering individuals to make informed decisions about their health. Diabetes education programs, support groups, and resources provide valuable information and support for managing the condition effectively.
Regular Healthcare Visits:
Routine visits to healthcare providers, including primary care physicians, endocrinologists, and diabetes educators, are essential for ongoing monitoring and management of diabetes. These visits allow for regular assessment of blood sugar control, medication adjustments, and screening for complications.
Lifestyle Modifications:
In addition to diet and exercise, other lifestyle factors can impact diabetes management. These include getting adequate sleep, managing stress levels, avoiding smoking and excessive alcohol consumption, and staying hydrated.
Awareness of Hypoglycemia and Hyperglycemia:
Understanding the signs and symptoms of both low blood sugar (hypoglycemia) and high blood sugar (hyperglycemia) is important for prompt intervention and prevention of complications. Treatment protocols for hypoglycemia (such as consuming fast-acting carbohydrates) should be readily accessible.
Foot Care:
People with diabetes are at increased risk of foot complications due to nerve damage (neuropathy) and poor circulation. Practicing good foot care, including daily inspection, proper footwear, and regular foot exams by healthcare providers, can help prevent foot ulcers and infections.
Management of Other Health Conditions:
Diabetes often coexists with other health conditions such as hypertension, dyslipidemia, and kidney disease. Managing these conditions through medication, lifestyle modifications, and regular monitoring is essential for overall health and wellbeing.
By addressing these additional aspects of diabetes management in conjunction with diet and exercise, individuals can take a comprehensive approach to managing their condition and reducing the risk of complications. It's important for individuals with diabetes to work closely with their healthcare team to develop a personalized treatment plan that addresses their unique needs and goals. With proactive management and support, it is possible to live a fulfilling life with diabetes while minimizing its impact on overall health.
Real-life examples illustrating the importance of diet, exercise, and other aspects of diabetes management:
Diet and Exercise:
Carbohydrate Management Example:
Sarah, diagnosed with type 2 diabetes, decides to focus on managing her carbohydrate intake. She starts replacing refined carbohydrates like white bread with whole grain options and incorporates more vegetables into her meals. As a result, she notices more stable blood sugar levels throughout the day.
Exercise Adherence Example:
John, who has type 1 diabetes, commits to a regular exercise routine consisting of brisk walks and strength training sessions at the gym. He sets reminders on his phone to stay consistent with his workouts. Over time, he experiences improved insulin sensitivity and better overall blood sugar control.
Other Aspects of Diabetes Management:
Medication Adherence Example:
Maria, diagnosed with gestational diabetes during pregnancy, diligently follows her healthcare provider's instructions for insulin injections. She maintains a log to track her medication doses and ensures she administers them at the recommended times each day, resulting in better blood sugar management for herself and her baby.
Regular Monitoring Example:
Tom, who has type 2 diabetes, uses a continuous glucose monitoring (CGM) system to track his blood sugar levels in real-time. By regularly reviewing his CGM data and discussing it with his healthcare provider during check-up visits, Tom can make timely adjustments to his diet, exercise, and medication as needed to maintain optimal blood sugar control.
Lifestyle Modification Example:
Emily, diagnosed with type 2 diabetes and high blood pressure, quits smoking and reduces her alcohol consumption. She also prioritizes getting enough sleep each night and practices stress-reduction techniques such as meditation and yoga. These lifestyle changes, along with dietary modifications and regular exercise, contribute to better overall health and improved diabetes management.
Foot Care Example:
David, who has had diabetes for several years, checks his feet daily for any signs of injury or infection. He wears comfortable, well-fitting shoes and socks to prevent blisters and sores. During his regular diabetes check-up appointments, his healthcare provider conducts thorough foot exams and provides guidance on proper foot care practices.
These real-life examples demonstrate how individuals can integrate various aspects of diabetes management into their daily lives to achieve better health outcomes and reduce the risk of complications. By taking a proactive approach and working closely with healthcare professionals, people with diabetes can effectively manage their condition and lead fulfilling lives.
Education and Support:
Diabetes Education Program Example:
After being diagnosed with type 1 diabetes, Mark attends a diabetes education program offered by his local hospital. Through the program, he learns about carbohydrate counting, insulin management, blood sugar monitoring, and strategies for preventing complications. Mark also connects with other individuals living with diabetes, forming a support network that provides encouragement and practical advice.
Regular Healthcare Visits:
Primary Care Physician Visits Example:
Lisa, who has type 2 diabetes, visits her primary care physician every three months for routine check-ups. During these visits, her physician monitors her blood sugar levels, reviews her medication regimen, and conducts screenings for complications such as diabetic retinopathy and kidney disease. By staying proactive with her healthcare, Lisa can address any concerns promptly and adjust her treatment plan as needed.
Awareness of Hypoglycemia and Hyperglycemia:
Hypoglycemia Management Example:
James, a college student with type 1 diabetes, experiences symptoms of hypoglycemia while studying in the library. He quickly recognizes the signs, including shakiness and sweating, and consumes a glucose tablet from his backpack to raise his blood sugar levels. James also informs his friends about his condition and teaches them how to help him in case of a severe hypoglycemic episode.
Management of Other Health Conditions:
Hypertension Management Example:
Sarah, who has type 2 diabetes and high blood pressure, takes prescribed medication to manage both conditions. In addition to medication, she focuses on lifestyle modifications such as reducing sodium intake, increasing physical activity, and maintaining a healthy weight. By effectively managing her hypertension, Sarah reduces her risk of cardiovascular complications associated with diabetes.
These additional real-life examples underscore the multifaceted nature of diabetes management and highlight the importance of addressing various aspects of the condition to achieve optimal health outcomes. By embracing a holistic approach that encompasses education, support, regular healthcare visits, awareness of blood sugar fluctuations, and management of comorbidities, individuals with diabetes can better control their condition and enhance their overall quality of life.
Conclusion
Diet and exercise are powerful tools in the management of diabetes. By making healthy dietary choices and incorporating regular physical activity into daily routines, individuals with diabetes can achieve better blood sugar control, maintain a healthy weight, and reduce the risk of complications. It's essential to work closely with healthcare professionals to develop a personalized plan that meets individual needs and goals. With dedication and consistency, lifestyle modifications can significantly improve the quality of life for those living with diabetes.
