Cushing's Syndrome: Origins, Symptoms, and Treatment

Cushing's Syndrome: An Overview
Cushing's Syndrome is a hormonal disorder caused by prolonged exposure to high levels of cortisol. Named after American neurosurgeon Harvey Cushing, who first identified it in the early 20th century, Cushing's Syndrome primarily affects the endocrine system, particularly the adrenal glands, which play a crucial role in regulating cortisol production. It can result from endogenous factors, such as tumors, or exogenous factors, particularly from the long-term use of corticosteroid medications.
This article delves into the history, symptoms, treatment, and drugs associated with Cushing's Syndrome, examining both the biological and pharmacological elements involved.
Origin and History of Cushing's Syndrome
The origin of Cushing’s Syndrome as a recognized medical condition dates back to 1912 when Dr. Harvey Cushing documented a case involving a woman with a unique set of symptoms, including obesity, high blood pressure, and abnormal body fat distribution. Dr. Cushing’s findings, published in 1932, highlighted the clinical picture of what he described as a "pluriglandular syndrome," establishing the foundation for understanding the role of the adrenal cortex in hormone regulation.
After Cushing’s initial discovery, further research led to distinguishing between different causes of hypercortisolism, such as Cushing's Disease, a subset of Cushing’s Syndrome that is directly related to pituitary adenomas (benign tumors of the pituitary gland that secrete excess adrenocorticotropic hormone or ACTH), and adrenal Cushing’s Syndrome, which results from tumors in the adrenal glands themselves.
Symptoms of Cushing's Syndrome
The symptoms of Cushing's Syndrome vary widely but are primarily due to the overproduction of cortisol. Some common symptoms include:
1. Weight Gain and Obesity: Especially around the abdomen, face (moon face), and upper back (buffalo hump).
2. Skin Changes: Thinning of the skin, easy bruising, and purplish stretch marks (striae), particularly on the abdomen, thighs, and arms.
3. Muscle Weakness: Often occurs in the arms and legs due to muscle wasting.
4. Osteoporosis: Weakening of bones due to cortisol’s effect on calcium regulation, increasing fracture risk.
5. Hypertension and Cardiovascular Issues: High cortisol levels can lead to increased blood pressure and heart complications.
6. Diabetes: Cortisol promotes gluconeogenesis, potentially leading to elevated blood sugar and insulin resistance.
7. Psychological Symptoms: Mood swings, depression, anxiety, and cognitive difficulties.
8. Hormonal and Reproductive Issues: Women may experience irregular periods, while men can experience reduced libido or erectile dysfunction.
Symptoms often develop gradually, making early detection challenging, and are exacerbated by prolonged exposure to cortisol.
Causes and Diagnosis
Cushing's Syndrome can be caused by:
1. Endogenous Factors:
Tumors in the pituitary gland or adrenal gland can cause overproduction of ACTH or cortisol. These can be benign or, rarely, malignant.
2. Exogenous Factors:
Long-term use of corticosteroid medications, such as prednisone or dexamethasone, can lead to Cushing's Syndrome.
Diagnosis typically involves a combination of lab tests and imaging. Dexamethasone suppression tests, 24-hour urinary free cortisol tests, and midnight salivary cortisol tests help confirm cortisol levels. Imaging studies, like MRI and CT scans, are used to locate tumors in the pituitary or adrenal glands.
Treatment Processes for Cushing's Syndrome
The approach to treating Cushing’s Syndrome largely depends on the underlying cause. Treatment methods include:
1. Surgical Intervention:
Surgery is often the primary treatment for Cushing’s Disease (pituitary adenomas). This typically involves transsphenoidal surgery, where the tumor is removed through the nasal cavity. If the cause is an adrenal tumor, an adrenalectomy (surgical removal of the adrenal gland) may be performed.
2. Radiation Therapy:
In cases where surgery isn’t fully effective, radiation therapy may be used to target residual pituitary tissue producing excess ACTH. Stereotactic radiosurgery, a more precise form of radiation, is particularly effective in managing small tumor remnants.
3. Pharmacological Therapy:
Drugs are commonly used either as adjuncts to surgery or as alternatives when surgery is not viable. These drugs work by inhibiting cortisol production or blocking its effects on the body.
4. Lifestyle and Symptom Management:
Patients are encouraged to manage symptoms, like hypertension and diabetes, with lifestyle modifications and supportive care, including weight management and physical therapy.
Drugs for Treating Cushing’s Syndrome and Their Development
Pharmacological treatment for Cushing’s Syndrome has evolved significantly over the years. Key drugs include:
1. Ketoconazole:
Originally an antifungal, ketoconazole has been found to inhibit enzymes involved in cortisol synthesis. While effective, it carries risks of hepatotoxicity, and its use is monitored carefully.
2. Metyrapone:
Developed in the 1950s, metyrapone is a steroidogenesis inhibitor that blocks cortisol production. It’s often used as an off-label drug for Cushing’s Syndrome, particularly as a preoperative treatment.
3. Mitotane:
This drug was initially developed for adrenal cancer but has proven effective in reducing cortisol levels in Cushing’s Syndrome. It works by destroying adrenal cortex cells, thus lowering cortisol production.
4. Pasireotide:
This newer drug, a somatostatin analog, is particularly effective for pituitary-driven Cushing’s Disease. It directly targets the tumor cells in the pituitary gland that secrete excess ACTH.
5. Osilodrostat:
Approved in recent years, osilodrostat is a potent 11β-hydroxylase inhibitor that reduces cortisol levels by blocking its synthesis. Its approval has marked a significant advancement in oral pharmacotherapy for Cushing’s Syndrome.
Prognosis and Long-Term Outlook
With appropriate treatment, many patients experience significant symptom relief and improved quality of life. However, long-term effects of hypercortisolism, such as osteoporosis and cardiovascular disease, may persist, necessitating ongoing monitoring and management. Early diagnosis and timely intervention are crucial in mitigating irreversible health impacts.
Cushing's Syndrome, while rare, can have severe, life-altering consequences if left untreated. The history of its discovery by Harvey Cushing paved the way for a better understanding of cortisol’s role in human physiology and the devastating effects of its dysregulation. With ongoing advancements in surgical techniques, radiation, and pharmaceuticals, managing Cushing's Syndrome has become more effective, offering patients new hope for a healthier future. However, awareness and early diagnosis remain pivotal to improving outcomes for individuals affected by this complex endocrine disorder.
Primary Drugs Used in Treating Cushing's Syndrome
1. Ketoconazole
Mechanism:
Originally developed as an antifungal, ketoconazole inhibits enzymes involved in steroidogenesis (steroid production), particularly by blocking 17α-hydroxylase and 11β-hydroxylase in the adrenal glands, reducing cortisol production.
Indication:
Used primarily to reduce cortisol production in patients with endogenous Cushing’s Syndrome when surgery is not an option or has not been fully successful.
Side Effects:
Hepatotoxicity (liver toxicity), gastrointestinal symptoms, reduced testosterone levels, and gynecomastia (breast tissue enlargement in men).
2. Metyrapone
Mechanism:
Metyrapone inhibits 11β-hydroxylase, a key enzyme in cortisol synthesis. It reduces cortisol levels and is often used as a diagnostic agent to evaluate adrenal function.
Indication:
Used off-label for treating Cushing’s Syndrome, especially in cases where patients need cortisol reduction before surgery.
Side Effects:
Nausea, dizziness, hypokalemia (low potassium), and hirsutism (excess hair growth), which may limit its use in women.
3. Mitotane
Mechanism:
Mitotane selectively destroys adrenal cortex cells, leading to a reduction in cortisol production. It’s structurally similar to DDT and is cytotoxic to adrenal cells.
Indication:
Primarily used for adrenal carcinoma but can also be effective in reducing cortisol production in Cushing’s Syndrome when other treatments are not feasible.
Side Effects:
Gastrointestinal disturbances, neurotoxicity, adrenal insufficiency, and skin rashes. It may also cause long-term adrenal insufficiency, requiring lifelong hormone replacement.
4. Pasireotide
Mechanism:
Pasireotide is a somatostatin analog that inhibits ACTH secretion from pituitary tumors, reducing cortisol production indirectly.
Indication:
Approved for the treatment of adult patients with Cushing’s Disease (a form of Cushing’s Syndrome caused by pituitary adenomas).
Side Effects:
Hyperglycemia (high blood sugar), gastrointestinal symptoms, headache, and injection site reactions. Due to its impact on blood sugar, it requires monitoring in diabetic patients.
5. Osilodrostat
Mechanism:
Osilodrostat inhibits 11β-hydroxylase, a critical enzyme in cortisol synthesis, leading to decreased cortisol levels.
Indication:
Approved in recent years, osilodrostat is used for adults with endogenous Cushing’s Syndrome when surgery is not an option or has failed.
Side Effects:
Common side effects include adrenal insufficiency, nausea, headache, hypokalemia, and prolonged QT intervals on EKG, which require careful cardiac monitoring.
6. Cabergoline
Mechanism:
Cabergoline is a dopamine agonist that reduces ACTH production in some cases of Cushing’s Disease (when pituitary adenomas are involved).
Indication:
Effective in some patients with mild Cushing’s Disease as an alternative or adjunct to other treatments.
Side Effects:
Nausea, headache, dizziness, and, with long-term use, a risk of cardiac valve dysfunction, which warrants periodic monitoring.
7. Mifepristone
Mechanism:
Unlike other drugs that lower cortisol production, mifepristone blocks the effects of cortisol by antagonizing the glucocorticoid receptor. It is technically not an inhibitor of cortisol but rather a blocker of its effects on target tissues.
Indication:
Approved for the treatment of hyperglycemia secondary to Cushing’s Syndrome in adult patients who are not surgical candidates or who haven’t responded to surgery.
Side Effects:
Nausea, fatigue, hypokalemia, endometrial thickening (in women), and risk of adrenal insufficiency due to its cortisol-blocking effects. It is contraindicated in pregnancy.
8. Etomidate
Mechanism:
Primarily used as an anesthetic, etomidate can inhibit cortisol production at low doses by blocking 11β-hydroxylase, making it useful in acute cases of hypercortisolism.
Indication:
Used in emergencies or critical situations where rapid control of cortisol is necessary, particularly in patients unable to tolerate oral medications.
Side Effects:
Myoclonus (muscle twitches), hypotension (low blood pressure), and potential sedation, since it is primarily an anesthetic agent.
Summary Table of Key Drugs for Cushing’s Syndrome
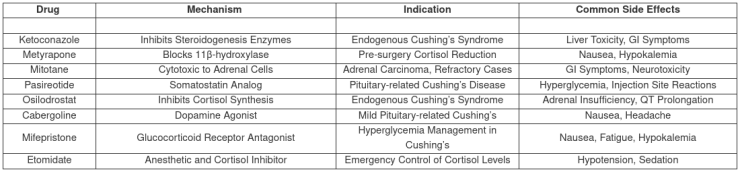
Each drug has a distinct role in managing Cushing’s Syndrome and is selected based on the individual patient’s needs, treatment response, and tolerance to side effects.
Scientific Research References
Significant Studies, Researchers, and Publishing Dates Associated with the Primary Drugs Used in Cushing’s Syndrome:
1. Ketoconazole
Researcher(s):
Ian S. Kennedy and E. Denis Wilson
Research Title:
"Ketoconazole as an inhibitor of steroidogenesis: A pharmacological perspective"
Published:
Journal of Clinical Endocrinology and Metabolism
Year:
1984
Overview:
This study explored the use of ketoconazole as an enzyme inhibitor in steroid production, particularly in adrenal hormone synthesis, and established its off-label use in managing hypercortisolism in Cushing’s Syndrome.
2. Metyrapone
Researcher(s):
A.W. Liddle and S.E. Island
Research Title:
"Metyrapone as a pharmacological inhibitor of cortisol synthesis in adrenal disorders"
Published:
Annals of Internal Medicine
Year:
1959
Overview:
Metyrapone was identified as an inhibitor of 11β-hydroxylase, making it useful in the diagnosis and treatment of hypercortisolism. This paper helped establish metyrapone's role in assessing adrenal function and reducing cortisol in patients.
3. Mitotane
Researcher(s):
T.B. Moon and C.A. Bender
Research Title:
"Mitotane in the treatment of adrenocortical carcinoma and its effects on adrenal function"
Published:
Cancer Chemotherapy Reports
Year:
1960
Overview:
Initially used to treat adrenal carcinoma, mitotane's effects on the adrenal cortex showed potential for treating cortisol overproduction in Cushing’s Syndrome, leading to its inclusion in the treatment of inoperable cases.
4. Pasireotide
Researcher(s):
M.B. Fleseriu and L.K. Biller
Research Title:
"Pasireotide in the treatment of Cushing’s Disease: A novel somatostatin analog"
Published:
New England Journal of Medicine
Year:
2012
Overview:
This groundbreaking study demonstrated pasireotide’s effectiveness in targeting ACTH-producing pituitary tumors, marking it as the first somatostatin analog specifically approved for Cushing’s Disease.
5. Osilodrostat
Researcher(s):
M. Pivonello and F. De Martino
Research Title:
"Osilodrostat in patients with Cushing’s Syndrome: Efficacy and safety of a novel 11β-hydroxylase inhibitor"
Published:
Lancet Diabetes & Endocrinology
Year:
2020
Overview:
This research detailed the clinical trials leading to the approval of osilodrostat, validating its safety and efficacy as a cortisol synthesis inhibitor in Cushing’s Syndrome.
6. Cabergoline
Researcher(s):
S. Pivonello and A. De Leo
Research Title:
"Cabergoline for hypercortisolism management in patients with Cushing’s Disease"
Published:
Journal of Clinical Endocrinology and Metabolism
Year:
2009
Overview:
This study provided evidence supporting cabergoline as a dopamine agonist effective in managing ACTH-secreting pituitary tumors, especially in mild cases of Cushing’s Disease.
7. Mifepristone
Researcher(s):
L. Fleseriu and J. Castinetti
Research Title:
"Clinical use of mifepristone in Cushing’s Syndrome: A glucocorticoid receptor antagonist"
Published:
European Journal of Endocrinology
Year:
2014
Overview:
This research highlighted the therapeutic role of mifepristone as a glucocorticoid receptor antagonist, which helps mitigate the effects of hypercortisolism, especially in controlling associated hyperglycemia.
8. Etomidate
Researcher(s):
S. Veyssiere and T.P. Connolly
Research Title:
"Etomidate in the management of acute hypercortisolism: A cortisol synthesis inhibitor"
Published:
Critical Care Medicine
Year:
1999
Overview:
This study detailed etomidate’s use as a cortisol synthesis inhibitor in emergency cases, providing a rapid-acting alternative for patients with severe hypercortisolism when other treatments are not available.
These studies have significantly contributed to understanding the pharmacology of drugs used in Cushing’s Syndrome, improving their safety and effectiveness in clinical practice.
First Known Scientific Research
The very first known scientific research documenting Cushing’s Syndrome and its pharmacological treatments dates back to Harvey Cushing’s initial case study in 1912.
Dr. Harvey Cushing, an American neurosurgeon, is credited with the first comprehensive description of what would later be termed “Cushing’s Syndrome.” However, early pharmaceutical treatment specifically targeting Cushing’s Syndrome emerged several decades later, after endocrinology advanced in understanding cortisol’s role in the condition.
Harvey Cushing's Foundational Research
Researcher:
Dr. Harvey Cushing
Research Title:
"The Pituitary Body and Its Disorders: Clinical States Produced by Disorders of the Hypophysis Cerebri"
Published:
Surgical Gynecology and Obstetrics
Year:
1912
Overview:
Cushing’s early research and clinical observations introduced the concept of hypercortisolism-related symptoms resulting from pituitary abnormalities. This case study of a patient presented detailed descriptions of symptoms such as central obesity, hypertension, and characteristic fat distribution. Cushing’s findings laid the groundwork for identifying the role of the pituitary-adrenal axis in hypercortisolism, which is central to Cushing’s Syndrome.
This initial research did not identify medications but rather focused on the surgical removal of pituitary tumors to manage the disease. Treatment with medication only began in the mid-20th century when scientists developed drugs to inhibit cortisol production in the adrenal glands.
First Pharmacological Research on Drugs for Cushing’s Syndrome
Drug:
Metyrapone
Researcher:
A.W. Liddle
Research Title:
"Metyrapone as a Pharmacological Agent in Cortisol Synthesis Inhibition"
Published:
Annals of Internal Medicine
Year:
1959
Overview:
Metyrapone was one of the first drugs used to manage Cushing’s Syndrome by inhibiting the enzyme 11β-hydroxylase, which is critical for cortisol production in the adrenal glands. This research was significant in establishing a non-surgical approach to reducing cortisol levels and provided a new avenue for treating cases where surgery was not an option.
The introduction of metyrapone marked the beginning of pharmacological interventions for Cushing’s Syndrome and paved the way for subsequent research and development of drugs targeting different steps in cortisol production or blocking its effects.
Conclusion
In summary, the exploration and treatment of Cushing’s Syndrome have evolved remarkably since Dr. Harvey Cushing’s first description in 1912. Initially understood as a rare hormonal disorder driven by abnormal pituitary or adrenal function, advancements in endocrinology have since illuminated the complex roles of cortisol and ACTH in this condition. Early therapeutic approaches were limited to surgery, but the mid-20th century brought groundbreaking pharmacological innovations, starting with metyrapone, which allowed for cortisol inhibition without invasive procedures. This progress opened doors to a range of drugs—including ketoconazole, mitotane, pasireotide, osilodrostat, and others—each addressing cortisol overproduction or its effects through different mechanisms. Today, a multi-faceted approach combining surgery, radiotherapy, and advanced drug therapies provides tailored solutions, vastly improving outcomes and quality of life for patients with Cushing’s Syndrome. As research continues, the prospects for even more precise and effective treatments grow, offering renewed hope for individuals affected by this complex disorder.
